Written by:
Melinda Craike
Bo Klepac, Victoria University
Mary Woessner, Victoria University
By Professor Melinda Craike, Dr Bo Klepac, and Dr Mary Woessner, Victoria University, Melbourne, Australia
Improving the uptake of research evidence in policy and practice is rarely straightforward – a challenge shared across many areas such as public health and sustainability. It is shaped by complex pathways involving the initiation, production, and dissemination of research, and is influenced by the actions of many actors within an evidence ecosystem. Among these, research funders hold a unique and often under-recognised power to shape whether, and how, research leads to societal impact.
Research doesn’t happen in a vacuum. It is part of a broad landscape, an evidence ecosystem, that brings together researchers, funders, policymakers, practitioners, and communities.
Funders shape research not just through WHAT they fund, but also HOW they fund it. The ways in which they design funding schemes, shape portfolios and reward outcomes, gives them a powerful role in influencing how research is conceived, conducted, and connected to the real world. But the potential of funders to enable societal impact often remains under-recognised.
In our recent Transforming Evidence blog, we identified several ‘funder influence mechanisms’ to describe the strategies, design choices, and operational levers that funders use to shape the production, translation, and use of research. We found that:
Funder influence mechanisms are important. They can affect who takes part in research, what questions are asked, and how results are used in policy and practice, ultimately shaping societal impact.
Examples include:
However, our initial look at the literature revealed a problem: there is no common language to describe these mechanisms. Without consistent definitions and classifications of funder influence mechanisms, it is difficult to evaluate strategies, compare findings, or build an evidence base on which work best.
Despite growing interest, there is currently no widely used framework to classify the mechanisms that funders use to influence societal impact. Creating such a classification system – essentially a structured “menu” of mechanisms grouped by common themes – could bring clarity and consistency to this growing field. This is not just an academic exercise; it offers clear, practical benefits.
A shared classification system provides a vocabulary and structure for understanding and improving the role of funders within the societal impact pathway.
A shared classification system of funder influence mechanisms could:
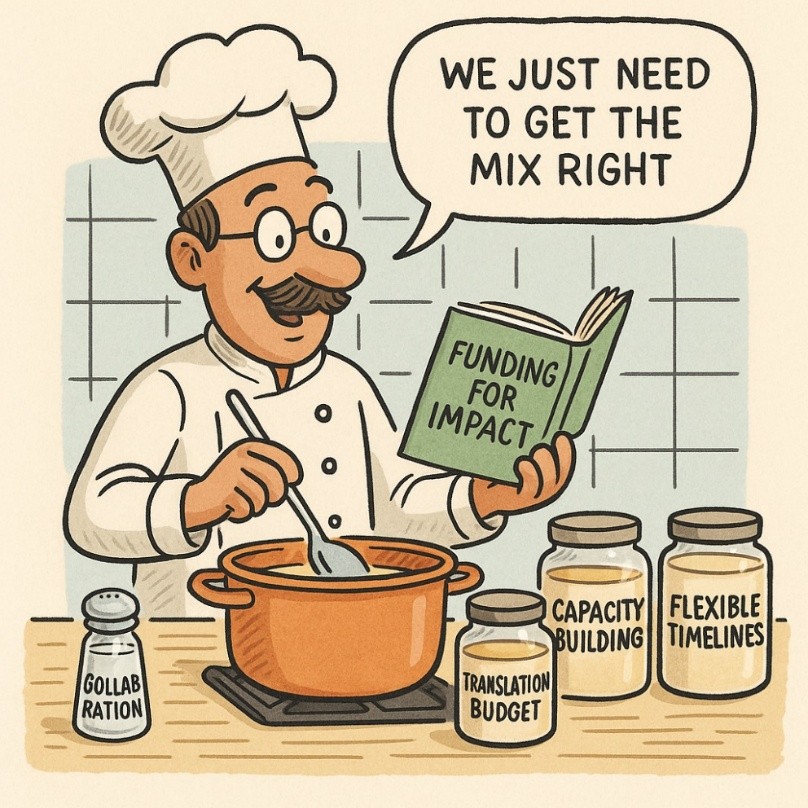
Illustration 1: A classification system of funder influence mechanisms would give funders a menu of mechanisms from which to select the right mix to achieve their funding goals. Image produced using Chat GPT
We are not starting from scratch – there is already work underway on strategies that public science funders and health funders are using to build on.
Figure 1 shows the beginnings of what a classification system of funder influence mechanisms, first introduced in our previous blog, might look like. It is based on an initial examination of the literature (see references below) to identify funder influence mechanisms, which we grouped into thematic domains.
Figure 1: Funder Influence Mechanisms: Example Classification System
We are keen to hear from funders, researchers, and other actors in the evidence ecosystem who are interested in co-developing and testing a classification system of funder influence mechanisms. If you are exploring new ways to strengthen the link between funding design and societal impact, we’d love to hear from you. Get in touch via Transforming Evidence or connect with us on LinkedIn: Melinda Craike, Bo Klepac, Mary Woessner.
About the Authors:
Melinda Craike is Professor of Physical Activity and Health and Associate Director, Research Engagement and Impact at the Institute for Health and Sport, Victoria University, Melbourne, Australia.
Mary Woessner is a Senior Lecturer of Clinical Exercise Science and Coordinator, Research Engagement and Impact at the Institute for Health and Sport, Victoria University, Melbourne, Australia.
Bo Klepac is a Senior Research Fellow at the Mitchell Institute, Victoria University, Melbourne, Australia.
Melinda Craike and Bo Klepac are the co-founders of Quality for Outcomes (www.qualityoutcomes.au) which helps prevention and health promotion teams strengthen quality, improve planning and evaluation, and achieve greater impact.
Abudu, R., Oliver, K., & Sealey, B. (2024). NORFACE evaluation for the Economic and Social Research Council. ESRC-03122024-NORFACE-Evaluation-Final-Report.pdf
Abudu, R., Oliver, K., & Boaz, A. (2022). What funders are doing to assess the impact of their investments in health and biomedical research. Health Research Policy and Systems, 20(1), 88. https://doi.org/10.1186/s12961-022-00888-1
Arnott, J. C., Kirchhoff, C. J., Meyer, R. M., Meadow, A. M., & Bednarek, A. T. (2020). Sponsoring actionable science: What public science funders can do to advance sustainability and the social contract for science. Current Opinion in Environmental Sustainability, 42, 38–44. https://doi.org/10.1016/j.cosust.2020.01.006
Baxter, H., Bearne, L., Stone, T., Thomas, C., Denholm, R., Redwood, S., Purdy, S., & Huntley, A. L. (2024). The effectiveness of knowledge-sharing techniques and approaches in research funded by the NIHR: A systematic review. Health Research Policy and Systems, 22(1), 41. https://doi.org/10.1186/s12961-024-01127-5
Beckett, K., Farr, M., Kothari, A., Wye, L., & le May, A. (2018). Embracing complexity and uncertainty to create impact: Exploring the processes and transformative potential of co-produced research through development of a social impact model. Health Research Policy and Systems, 16(1), 118. https://doi.org/10.1186/s12961-018-0375-0
Boulding, H., Kamenetzky, A., Ghiga, I., Ioppolo, B., Herrera, F., Parks, S., Manville, C., Guthrie, S., & Hinrichs-Krapels, S. (2020). Mechanisms and pathways to impact in public health research: A preliminary analysis of research funded by the National Institute for Health Research (NIHR). BMC Medical Research Methodology, 20(1), 34. https://doi.org/10.1186/s12874-020-0905-7
Guthrie, S., Bienkowska-Gibbs, T., Manville, C., Pollitt, A., Kirtley, A., & Wooding, S. (2015). The impact of the National Institute for Health Research Health Technology Assessment programme, 2003–13: A multimethod evaluation. Health Technology Assessment, 19(67), 1–291. https://doi.org/10.3310/hta19670
Guthrie, S., Kirtley, A., Garrod, B., Pollitt, A., Grant, J., & Wooding, S. (2016). A “DECISIVE” approach to research funding: Lessons from three Retrosight studies. RAND Corporation. https://www.rand.org/pubs/research_reports/RR1132.html
Klepac, B., Krahe, M., Spaaij, R., & Craike, M. (2023). Six public policy recommendations to increase the translation and utilization of research evidence in public health practice. Public Health Reports, 138(5), 715–720. https://doi.org/10.1177/00333549221129355
McLean, R. K., Graham, I. D., & Tetroe, J. M. (2018). Evaluation of funding efforts to promote and/or support research impact. Health Research Policy and Systems, 16(1), 1–8. https://doi.org/10.1186/s12961-018-0316-y
Sibbald, S. L., Tetroe, J., & Graham, I. D. (2014). Research funder required research partnerships: A qualitative inquiry. Implementation Science, 9(1), 176. https://doi.org/10.1186/s13012-014-0176-y
Smits, P. A., & Denis, J. L. (2014). How research funding agencies support science integration into policy and practice: An international overview. Implementation Science, 9(1), 28. https://doi.org/10.1186/1748-5908-9-28
van der Linden, B., Dunham, K. M., Siegel, J., et al. (2022). Health funders’ dissemination and implementation practices: Results from a survey of the Ensuring Value in Research (EViR) Funders’ Forum. Implementation Science Communications, 3(1), 36. https://doi.org/10.1186/s43058-022-00273-7